Introduction
Did you know that over one-third of the adult population has advance directives in the USA? Based on several studies, almost 37% of adults in America had completed advance directives for end-of-life care. If you wonder what an advance directive is, it is a legal document that layouts the kind of health care you prefer if you become incapacitated to make any decisions or speak for yourself. It does not have to be something you only consider when you get old or need nursing home level care. Many younger adults are considering this, too, since you can never predict a medical crisis, and it can happen at any point in your life.
Before creating an advance directive, you should talk about your medical choices and plans with your family, healthcare team, or anyone you consider trustworthy. You can discuss the decisions that might need to be made ahead of time and also whom you want to make those decisions for you if you are unable to do so. This way, an advance directive may assist your loved ones and physicians in making explicit judgments regarding the kind of care you want in the future.
What is an Advance Directive?
An advance directive is a legally binding document regulated by state laws. Advance directives are subject to The Patient Self-Determination Act (PSDA), 1990, a federal law that encourages individuals to plan in advance about their preferred medical care in case they become incapable of making decisions. The PSDA requires long-term care facilities to inform residents about their decision-making rights, recognize and honor their wishes, and not discriminate against their advanced directives.
However, the rules may vary from state to state. While some states may have flexible rules, some may follow very strict regulations. Your medical team’s special actions or emergency care may be part of these medical decisions. However, you may require clear evidence of your wishes or a legally designated decision-maker.
Advance directives solely relate to medical decisions and have no bearing on financial or financial decisions. Advance directives are governed by different legislation in different states. Talk to your doctor (or a lawyer) about completing an advance directive while you’re still well, in case you become too ill or unable to make medical decisions in the future.
Benefits of Advance Directives
Every state recognizes advance directives, and millions of people in the United States have them in their medical files. In addition, health-care providers, attorneys, hospice workers, and retiree organizations all support them.
In the event that you become disabled and therefore unable to communicate, an advance directive is a simple, easy document that allows you to convey your preferences. The form allows you to select someone else, such as a family member or close friend, to speak for you if you are unable to do so or speak for you at a specific time or in a particular circumstance.
A proper and open conversation is where it all begins. It may not be enjoyable, but it is crucial for you and your family’s well-being. If you haven’t made these decisions yet, they may be made for you by a bereaved loved one.
Today, people with life-threatening illnesses have a wide range of alternatives, from cutting-edge medical therapies to palliative care. You can tell doctors what you want and don’t want while you’re still alive by filling out an advance directive. When you have an advance directive, you may typically avoid:
- Unnecessary pain
- Unhelpful procedures
- Unwanted hospitalization
Where to Find an Advance Directive Form?
A list of advance directive forms for each state is available from the National Hospice and Palliative Care Organization. We recommend visiting your state government’s website for the latest up-to-date forms. You can quickly access all state and territorial government websites in the USA. Gov. Additionally, you can get free printable advanced directives forms of each state here.
What to Include in Your Advance Directive?
- Your healthcare agent’s or proxy’s name, address, and phone number.
- Answers to specific questions regarding how you want to be cared for if you become unable to communicate. From state to state, the paperwork and questions asked to differ.
- If your state requires it, the names and signatures of witnesses to your advance directive signing.
- If your state requires it, the signature and seal of a notary public.
4 Types of Advance Directives for Seniors
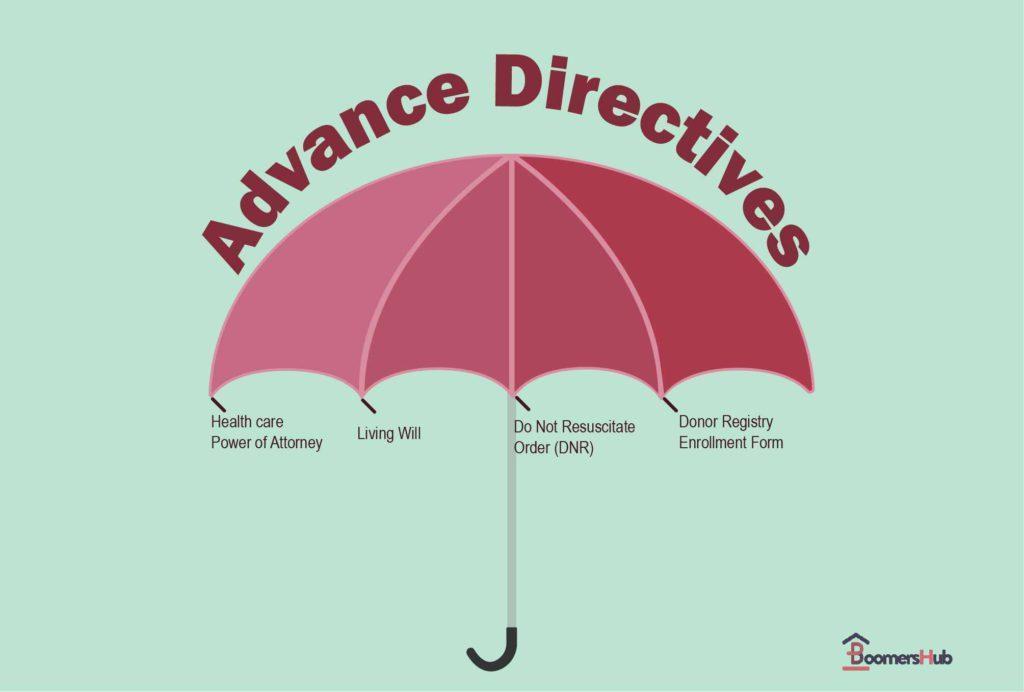
There are several different formats for advance directives. Some are designed by lawyers or even the patients themselves, while others follow state-mandated forms. State laws and courts decide the validity of these documents. Advance directives are legal in every state and the District of Columbia.
1. The Living Will
A living will is one of the many types of wills. It is a legal document that specifies certain future health-care decisions only if a person is unable to make them on their own. For example, a living will is only utilized near the end of life if a person is terminally ill (cannot be healed) or permanently unconscious. In these circumstances, the person’s living will specify the type of medical treatment he or she would choose. It can determine the circumstances under which a life-extension attempt should begin or end. This includes, but is not limited to, dialysis, tube feedings, and other forms of life support (such as the use of breathing machines).
You might have questions about how to handle certain medical emergencies or end-of-life decisions. You should talk these things through with your doctor, but here are some basics you can decide on ahead of time:
Cardiopulmonary Resuscitation (CPR)
Cardiopulmonary resuscitation (CPR) restarts the heart when it has stopped beating. Determine if and when you would want to be resuscitated by CPR or by a device that delivers an electric shock to stimulate the heart.
Mechanical Ventilation
Mechanical ventilation is a life-sustaining treatment that involves using a machine to assist with breathing. It is typically used when a person’s respiratory system is failing. Consider if, when and for how long you would want to be placed on this machine.
Tube Feeding
Tube feeding supplies the body with nutrients and fluids intravenously or via a tube in the stomach. If you are considering tube feeding, talk to your doctor to learn more about the potential risks and benefits. They can help you make an informed decision about whether or not tube feeding is right for you.
Dialysis
When kidney function begins to decline, waste starts to build up in the blood. Dialysis is a treatment that helps to remove those wastes and manage fluid levels in the blood. The decision of whether or not to receive dialysis is a personal one, and there are many factors to consider. These include your overall health, life expectancy, treatment preference and quality of life.
Antibiotics or Antiviral Medications
As anyone who has ever been ill knows, infections can be miserable. Antibiotics and antiviral drugs can be effective at treating these infections, but they also come with a risk of side effects. For people who are near the end of life, the decision of whether or not to treat an infection aggressively can be a difficult one.
Comfort Care (Palliative Care)
Comfort care, also known as palliative care, focuses on providing relief from symptoms and pain without necessarily trying to cure the underlying cause of the condition. Comfort care can be used in conjunction with other treatments or it can be provided as the sole form of treatment, depending on the patient’s preferences. Some common interventions used in comfort care include providing pain medication, ensuring adequate hydration, and avoiding invasive tests or treatments. In some cases, comfort care may also involve allowing the patient to die at home rather than in a hospital setting.
Organ and Tissue Donations
When making the decision to donate organs or tissues, consider the implications for your health care. If you are on life-sustaining treatment, you will need to be kept on this treatment until the procedure is complete. This can be confusing for your healthcare agent, so it is vital to state in your living will that you understand the need for this temporary intervention. By doing so, you can help to ensure that your wishes are carried out in the event of your untimely death.
2. Durable Power of Attorney (DPOA)
A DPOA for health care is also known as medical power of attorney. A POA is a legal instrument in which you choose someone to act as your proxy (agent) for all health-care decisions if you become unable to do so. Before a medical power of attorney is instated, a person’s doctor must declare that the person cannot make their own medical decisions.
If you become unable to make health-care decisions for yourself, your proxy or agent can talk with your health-care team and other caregivers on your behalf and make decisions based on the desires or orders you provided before. If you do not express your intentions in a certain situation, your agent will decide based on their belief about what you would want. Your proxy (agent) will no longer be able to make medical decisions on your behalf if you regain the ability to make your own decisions.
3. POLST (Physician Orders for Life-Sustaining Treatment)
A POLST form can also express health-care preferences, but it is not an advance directive. For example, a very ill individual can fill out a POLST form with a list of specific medical orders and have their health care professional sign it. In an emergency, a POLST form outlines your wishes, such as whether to do CPR (cardiopulmonary resuscitation), go to the hospital, be placed on a breathing machine if necessary, or stay put and be kept comfortable.
A qualified medical team member, such as your doctor, must sign the POLST form. Paramedics and EMTs (Emergency Medical Technicians) are unable to use advance directives, although they can use a POLST form. If you don’t have a POLST form, emergency professionals are obligated to provide you with every treatment necessary in order to save your life.
4. Do Not Resuscitate (DNR) Orders
If you have a Do Not Resuscitate order, nothing will be done to try to keep you alive if you cease breathing or your heart stops. You can have a DNR order added to your medical record if you are in the hospital. Only request this if you do not want the hospital professionals to attempt to resuscitate you if your heart or breathing stops. You may need to inquire each time you go to the hospital because certain hospitals demand a fresh DNR order each time you are hospitalized. However, keep in mind that this DNR order is only valid while you are hospitalized. It’s a different story outside the hospital.
Which Advance Directive Type Should I Choose?
Though there are different forms of advance directives, which type of advance directive you should choose depends on many factors such as health changes, a sudden diagnosis, change of preference, etc. So, it is best that you check with your physician about your present health condition and plan accordingly. For example, if you have high blood pressure with a risk of stroke or any kidney complications, then make sure you mention treatment decisions such as CPR and Dialysis in your living will.
Many choose the medical power of attorney as their preferred advance directive. One reason is that it makes your health-care wishes known and designates a responsible person to take the necessary decisions. In some states, family members automatically get designated if a person is unable to speak for themselves.
How Much Does an Advance Directive Cost and Where Do I Sign One?
An advanced directive costs around $250 to $500 if drafted by an attorney. However, one can write their living will absolutely free of charge. But some states might have rules that require the document to be witnessed by a notary, while some may not make it mandatory. In that case, it might cost some $20-$30 extra fees.
Advance directive forms can be created by the person himself or can be downloaded from online websites. Also, almost every state has advance directive forms on their website’s resources section. Another way is to ask your healthcare provider or existing attorney to prepare the document for you.
Conclusion
End-of-life planning is never easy, but it’s important to have a plan in place. Advance directives can help make sure your wishes are known and respected if you become unable to speak for yourself. If you haven’t created an advance directive yet, we encourage you to do so today. It could be the most important thing you ever do for yourself and your loved ones.
If you have any additional questions or would like to discuss your specific situation, please don’t hesitate to reach out to us. Call us at +(877) 409-0666 or email at info@boomershub.com. We would be happy to help!
Frequently Asked Questions Related to Advanced Directives
What percentage of Americans have an advance directive?
According to a new study of recent studies, about 37% of Americans have advanced directives for end-of-life care in the event that they become seriously ill or unable to make health-care decisions.
Should everyone have an advance directive?
An advance directive is a legal instrument that allows you to declare your health care and end-of-life desires ahead of time. An advance directive should be on file for everyone above 18.
What happens if you don’t have an advance directive?
If you didn’t create an advance directive and became unable to make medical decisions on your own, you may be offered medical treatment that you don’t want. In addition, if you don’t have an advance directive, the doctor may inquire about your care with your family.
What are end-of-life Decisions?
End-of-life decisions are ones you can make now about how you want to be cared for and treated as you approach death. Accepting or refusing treatments that could prolong your life is one example of an end-of-life decision.
What does Terminal condition mean?
A terminal illness has the potential to take one’s life away. Advanced malignancies, multiple organ failure, and some major heart attacks and strokes are all examples of a terminal illness.
When should I prepare an advance directive?
Creating an advance directive before you need it is the ideal time to do it. In other words, it is best to prepare the advanced directive before you get too ill to make decisions on your health-care treatment.
Do I need legal help to create my advance directive?
Although an attorney can be beneficial, most people do not require one to draft an advance directive. However, some states will ask you to fill out the paperwork with specific requirements. Speak with your medical staff to see if they can assist you in drafting an advance directive. There may also be sample forms and instructions available that comply with your state’s laws.
Can I have an advance directive in more than one state?
The majority of states use their own set of guidelines for what constitutes a legitimate advance directive. Some states will accept an out-of-state directive if it complies with the state’s legal standards. If you want to have one in more than one state, you should see a lawyer to avoid complications.
Can I have a durable power of attorney and a living will for health-care?
Yes, you can have a durable power of attorney and a living will for healthcare. However, if you have both of these documents, make sure they don’t contradict each other so that your wishes are clearly stated.
Who Can Be My Attorney-in-fact or Power of Attorney Under the Law?
Usually, an Attorney-in-fact or Power of Attorney has to be an acquaintance, an agent, a friend, or a beneficiary’s family member under US law. Whomever that person might be, he or she needs to be someone the beneficiary can fully trust, and they must be legally designated by the individual. Some states may have very specific rules for who qualifies as an Attorney-in-fact. So, it’s recommended to check out the state-specific guidelines before choosing an Attorney-in-fact.
